 Centers for Disease Control & Prevention Combating Risk Increases to Men Who Have Sex with Men HIV and STDs on the Rise in Cities, Say Recent CDC Reports |
|
Compiled by GayToday Courtesy of the Centers for Disease Control
 Recent data document disturbing increases in sexual risk taking among men
who have sex with men (MSM) in a growing number of cities in the United
States; a rise in sexually transmitted diseases (STDs), such as syphilis,
gonorrhea, and chlamydia; and a reported increase in the estimated HIV
incidence among MSM in San Francisco (CDC, Oct 2000; Denning et al., 2000,
San Francisco Dept. of Public Health).
Recent data document disturbing increases in sexual risk taking among men
who have sex with men (MSM) in a growing number of cities in the United
States; a rise in sexually transmitted diseases (STDs), such as syphilis,
gonorrhea, and chlamydia; and a reported increase in the estimated HIV
incidence among MSM in San Francisco (CDC, Oct 2000; Denning et al., 2000,
San Francisco Dept. of Public Health).
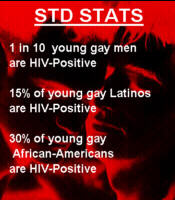
High rates of co-infection with HIV have been documented among MSM infected with these other STDs (CDC, Oct 2000; CDC MMWR, 1999). STD outbreaks in several major cities across the U.S. have shown that 25-73% of MSM with syphilis and 25-54% of MSM with gonorrhea are co-infected with HIV (CDC, Oct 2000). Despite significant declines in HIV infection rates among MSM since the early years of the epidemic, MSM continue to be the group at highest risk for HIV, accounting for an estimated 42% of all new infections in the United States (CDC, 2000). Young MSM, African-American MSM, and Latino MSM are at particularly high risk for HIV infection. In a recent study of young MSM in seven U.S. cities [INCLUDING BALTIMORE], more than one in ten young MSM were HIV infected, with infection rates of 15% among young Latino MSM and 30% among young African American MSM (Valleroy, 2001). Recent data on rates of HIV, STDs, and risk behaviors among MSM indicated that these men are at alarming and increasing risk for HIV infection. Given the high prevalence of HIV infection within MSM communities, relatively small increases in the rate of high-risk sexual behavior can rapidly produce significant increases in new HIV infections (CDC, Oct 2000; Wolitski et al., 2001). Without immediate action by MSM and the public health community, the gains made in fighting the HIV epidemic will likely be lost. Based on consultations with MSM community representatives and public health leaders held in October 2000 and February 2001, CDC has developed this Public Health Alert to communicate the urgent HIV and STD prevention needs of MSM and to provide technical guidance on immediate steps to address those needs. What has changed for MSM, and why are these trends of urgent concern? Several factors have contributed to changes in the HIV and STD prevention environment for MSM including the following:
 Optimism about New Therapies. The availability of effective antiretroviral
therapy and the fact that HIV-positive people are living longer and
healthier lives have created a false perception that HIV is no longer a
major health threat and helped to create a sense among some MSM that the
"crisis" of HIV is over (Stall, 2000). Some incorrectly believe that a
reduced viral load means that someone is no longer infectious, which has
made some MSM less vigilant about maintaining safer sexual practices
(Kravcik et al., 1998). However, the fact remains that despite important
medical advances, HIV remains an infectious, life-threatening disease that
requires complex, costly, and difficult treatment regimens that do not work
for everyone.
Optimism about New Therapies. The availability of effective antiretroviral
therapy and the fact that HIV-positive people are living longer and
healthier lives have created a false perception that HIV is no longer a
major health threat and helped to create a sense among some MSM that the
"crisis" of HIV is over (Stall, 2000). Some incorrectly believe that a
reduced viral load means that someone is no longer infectious, which has
made some MSM less vigilant about maintaining safer sexual practices
(Kravcik et al., 1998). However, the fact remains that despite important
medical advances, HIV remains an infectious, life-threatening disease that
requires complex, costly, and difficult treatment regimens that do not work
for everyone.
Prevention Burnout. Evidence of increasing risk behaviors among MSM underscores the difficulty of sustaining behavior change over a lifetime in any population. Twenty years into the HIV epidemic, many older men who adopted safer sex practices in response to the initial health crisis are finding it difficult to maintain these practices indefinitely ("prevention burnout"). Meanwhile, younger MSM - many of whom have never been personally affected by HIV - are also finding it challenging to practice safer sex every time. The Changing Face of the Epidemic. HIV/AIDS has had a disproportionate impact on racial/ethnic minority MSM, especially African Americans and Hispanics (CDC, MMWR, 2000). Race/ethnicity itself is not a risk factor for HIV infection; however, among racial/ethnic minority MSM, social and economic factors including homophobia, high rates of poverty and unemployment, and lack of access to prevention services and health care may serve as barriers to receiving HIV prevention information or accessing HIV testing, diagnosis, and treatment (ibid). Immediate Action Steps Are Needed Action is needed from national public health leaders, state and local health departments, HIV Prevention Community Planning Groups (CPGs), community-based organizations (CBOs), regional and national non-governmental organizations, and the MSM community itself. Comprehensive, community-specific strategies must be developed immediately to reduce HIV, STD, and viral hepatitis transmission and to improve health outcomes among MSM. Comprehensive strategies must include the following components: A Focus on Monitoring and Responding to Emerging Trends
An Assessment of HIV/STD Testing Approaches Health departments and CBOs should develop strategies to increase knowledge of HIV status among MSM. These strategies should: Ensure that anonymous HIV testing is readily available; Work with MSM communities to develop valid messages that stress the client benefits of HIV and STD testing; Make sure that private practitioners and social service organizations in communities have up-to-date information about HIV and STD testing services; Expand neighborhood and community-based voluntary HIV and STD testing (e.g., bars, bath houses, and special community events); Increase routine, voluntary HIV testing in STD clinics; and Increase routine, voluntary, HIV and STD testing in settings such as community health centers and hospital emergency rooms. Strategies are needed to increase the proportion of HIV-infected MSM who are linked to appropriate care and prevention services. Health departments and CBOs should enhance linkages to organizations that provide HIV-related care, so that men who test positive are successfully referred into care networks that are sensitive and attuned to their prevention needs. Health departments should evaluate whether current HIV and STD counseling, testing, and partner notification activities are reaching MSM. Health department staff should ensure, through training and ongoing quality assurance monitoring, that the counseling provided is "client-centered" (i.e., it reflects the needs and priorities of MSM clients). Clinicians should encourage and provide easy access to routine, voluntary HIV and STD prevention, testing, and treatment, including immunization for hepatitis A and B. Clinicians caring for HIV-infected and at-risk MSM should: Conduct routine sexual risk assessment; Update counseling messages; Obtain training at STD/HIV prevention training centers or other institutions. A Mechanism to Target Programs, Tailor Messages, and Create Linkages Health departments should better integrate HIV and STD prevention and care systems. This integration is critical because STDs are more than "markers" of risk behavior; they are biological co-factors that facilitate transmission and acquisition of HIV at least two- to five-fold (Fleming and Wasserheit, 1999). Both MSM and their care providers must be given the information to help them understand that in the AIDS era, other STDs are a major threat to health because these diseases serve as potential pathways to HIV infection. Health departments should address issues related to access to and quality of STD clinical services and should use surveillance systems to monitor STD and HIV trends (CDC Strategic Plan, 2000; CDC, 1998). Because many MSM lack key information about STDs, it is essential that health departments, CBOs, and clinicians incorporate information about STDs in all programs addressing HIV prevention for MSM and ensure that prevention programs are linked to STD screening and treatment (Ciesielski et al., 2000). Prevention programs must be culturally sensitive and appropriate to the language competency of the target population. Health departments should also strengthen liaisons with clinicians in private practice to make sure that they have accurate and up-to-date information about HIV and STDs among MSM. Prevention and outreach for HIV-positive MSM are critical. Prevention messages and intervention programs directed to men who are HIV-positive should be considered essential parts of outreach and intervention efforts for MSM. Messages targeting HIV-positive MSM should build on the sense of personal ownership for protecting others that many men already have and should reinforce the importance of having safer sex and protecting their own health. All clinical settings (including health department facilities, CBOs, primary care centers, and drug treatment facilities) should provide prevention services and referrals to care for HIV-infected persons (IOM, 2000). Prevention and outreach for HIV-negative MSM are also critical. Prevention messages and intervention programs aimed at men who are HIV-negative should help encourage a sense of responsibility and community, instilling the idea that it is everyone's responsibility to remain HIV-negative and assist others in maintaining safer sexual practices. Messages should be crafted in partnership with MSM community representatives and they should underscore the value of remaining HIV-negative, knowing one's HIV status, and encouraging others to know their status. Links exist between racism and homophobia and HIV risk behaviors and infection (Ross and Kelly, 2000). A tremendous stigma remains associated with acknowledging gay and bisexual activity in society; this stigma has had an impact on funding, service delivery, and prevention program implementation. All programs and messages targeting MSM should address the impact of homophobia and racism on HIV transmission. Health departments, CBOs, and clinicians should ensure programs, services, and messages are not provided in a racist or homophobic manner. Health departments should provide diversity training for their staff and others working with MSM in the community, and should seek out the involvement of diverse racial and ethnic perspectives. Health departments and CBOs should frame prevention programs and messages for MSM in the context of gay male health (Stall et al., 2000). Interventions should frame HIV/STD prevention messages in the context of other important MSM priorities and needs and be consistent with the principles of sound health promotion programs. These messages should be crafted in partnership with members of the MSM community, use language that is understandable to clients, and be available in clinical settings serving MSM, as well as in venues where MSM congregate or engage in high-risk behaviors. Health departments and CBOs should evaluate community- and individual-level interventions in their community to ensure they address the epidemic's changing dynamics (e.g., advent of new therapies). Interventions need to be better integrated into service programs for at-risk MSM (e.g., mental health and substance use treatment programs and outreach programs in social venues) to reflect the lives of MSMs and address factors that facilitate HIV exposure (Ross and Kelly, 2000). Health departments and CBOs should create mechanisms for MSM community input and conduct ongoing program evaluation. Health departments should develop and strengthen relationships with organizations serving MSM and enhance the capacity of these organizations to develop, implement, and evaluate interventions. Members of the MSM community should be encouraged to actively participate in prevention planning activities, including CPGs. Health departments, CBOs, and clinicians should develop warnings to advise MSM against using nonoxynol-9 (N-9) as a rectal microbicide. Recent data indicate that N-9 may increase the risk of HIV transmission during vaginal intercourse (van Damme, 2000). Although similar studies have not been performed among MSM using N-9 during anal intercourse, we do know that N-9 can cause damage to the cells lining the rectum - thus providing a portal of entry for HIV and other sexually transmissible agents (Phillips et al., 2000). Therefore, CDC has gone on record advising against the use of N-9 as a microbicide during anal intercourse. It should be noted that the level of N-9 used to lubricate condoms is much lower than the level found to be harmful in the van Damme study. If given the choice, condoms without N-9 lubrication would be desirable, but a condom lubricated with N-9 is clearly preferable to using no condom at all. HIV and STD programs and clinicians should actively educate MSM about this information. Resources CDC HIV Prevention Strategic Plan. CDC, in consultation with numerous partners, recently developed a strategic plan designed to cut the number of new HIV infections in the U.S. in half by 2005, from 40,000 annually to 20,000. One of the high priority objectives in the plan calls for an increase in the proportion of MSM who consistently engage in behaviors that reduce the risk of HIV acquisition or transmission. The strategies listed under this objective (see Goal I, Objective 2), along with other information contained in the plan may be useful for program planning purposes. Copies of the strategic plan are available at www.cdc.gov/nchstp/od/news/prevention.pdf or at NPIN: www.cdcnpin.org (1-800-458-5231). This Public Health Alert will be supplemented by a longer technical guidance document that will include long-term strategies and guidance for addressing the prevention needs of MSM. It will be released in summer 2001. To access this and other CDC information on HIV and STDs on the Internet, please refer to: NCHSTP: www.cdc.gov/nchstp/od/nchstp.html References Centers for Disease Control and Prevention. Consultation on recent trends in STD and HIV morbidity and risk behaviors among MSM. Atlanta, GA. October 30-31, 2000, Meeting Report. Centers for Disease Control and Prevention: HIV/AIDS among racial/ethnic minority men who have sex with men-United States, 1989-1998. MMWR 2000; 49:4-11. Centers for Disease Control and Prevention. HIV/AIDS surveillance report 2000; 12. Centers for Disease Control and Prevention. HIV prevention strategic plan through 2005. 2001. Centers for Disease Control and Prevention. HIV prevention through early detection and treatment of other STDs, United States. MMWR 1998;47 (no. RR-12) 1-12. Centers for Disease Control and Prevention. Resurgent bacterial sexually transmitted disease among men who have sex with men--King country, Washington, 1997-1999. MMWR Morb Mortal Wkly Rep 1999 Sept 10, 48(35):773-777. Ciesielski C, Zajackowski M, Flynn J, Swanson F. Knowledge and awareness of syphilis among attendees of the international Mr. leather competition. Oral presentation. National STD prevention conference, Milwaukee, WI. December 2000. Denning PH, Nakashima AK, Wortley P. Increasing rates of unprotected anal intercourse among HIV-infected men who have sex with men in the United States. Oral presentation. 13th international AIDS conference, Durban, South Africa. July 2000. Fleming DT, Wasserheit JW. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999; 75(1):3-17. Institute of Medicine, National Academy of Sciences. No time to lose: getting more from HIV prevention. Washington, DC: National Academy Press, 2000. Kravcik S, Victor G, Houston S, Sutherland D, Garber GE, et al. Effect of antiretroviral therapy and viral load on perceived risk of HIV transmission and the need for safer sexual practices. JAIDS 1998; 19:124-129. Phillips DM, Taylor CL, Zacharopoulos VR, Maguire RA. Nonoxynol-9 causes rapid exfoliation of sheets of rectal epithelium. Contraception 2000; 62: 149-154. Ross MS, Kelly JA. Interventions to reduce HIV transmission among homosexual men. In: Peterson, DiClemente CC, eds. Handbook of HIV prevention. New York: Kluwer Academic/Plenum Publishers, 2000: 201-216. Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The gay '90s: a review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS 2000;14(suppl3): S1-S14. Valleroy L et al. High HIV and risk behavior prevalence among 23-29 year old men who have sex with men in 7 US cities. Abstract 211. 8th conference on retroviruses and opportunistic infections, Chicago, IL. February 2001. van Damme L. Advances in topical microbicides. Oral presentation. 13th international AIDS conference, Durban, South Africa. July 2000. Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence in the HIV epidemic among men who have sex with men? Am J Public Health (in press, June 2001). |

